General FAQ
Have a question about a specific hip or knee surgery? Visit our patient education section for information and answers to common questions about hip and knee procedures.
General Questions
- Do you perform “minimally invasive” or “MIS” procedures?
- How long before I can walk?
- How long will I need to stay in the hospital?
- Can you tell me about surgery at the Munster Specialty Surgery Center?
- Can you tell me about surgery in Pleasant Prairie WI at North Shore Surgical Suites?
- What type of anesthesia is used?
- Will my muscle be cut at the time of my hip or knee replacement?
- Why do you recommend against going to a rehabilitation facility after surgery?
- I have diabetes. Will this affect my surgery?
- I am overweight. Will this affect my surgery?
- How long will my replacement last?
- Where do you perform surgery?
- If I have arthritis of both hips or knees, can I do them both at the same time?
- How long will I be in the operating room?
- I am not interested in surgery and want to explore non-operative treatment for my arthritis such as an injection into the joint and the use of medication and physical therapy. Should I come in to see Dr. Della Valle?
- Will I be asked to participate in any research studies?
- Are there any questions I am forgetting to ask?
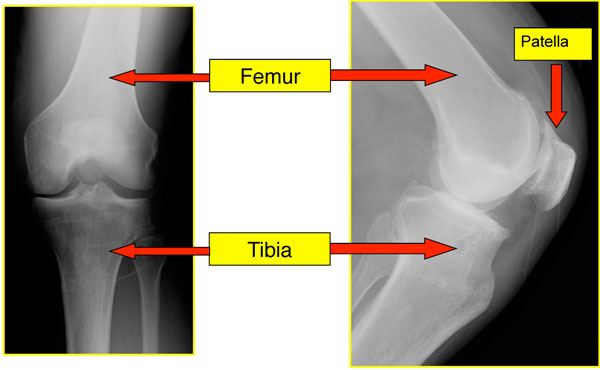
Basic Knee Anatomy
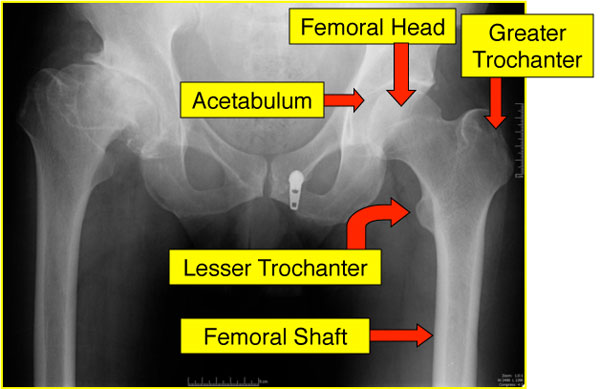
Basic Hip Anatomy
Do you perform “minimally invasive” or “MIS” procedures?
This is among the most common questions patients ask, and it is complicated to answer. First, there is no true medical or scientific definition of a “minimally invasive procedure”. To be honest, I don’t really like the term because it can mean so many different things to different people. For example, we perform a lot of partial knee replacements. Partial knee replacements involve less bony work inside the knee and hence you might consider that “less invasive”. We also perform hip resurfacing which takes away less bone but require a larger skin incision; does that mean it is less invasive or more invasive?
Further, the operations we perform have real risks associated with them and we prefer patients to be realistic and informed about the surgeries they are having as opposed to “minimizing” these issues. At the end of the day, I think what most people want (and what I would want for myself or my family) would be a procedure that is safe, associated with minimal pain and a quick recovery. The trick is, how to make that happen and again, do so safely. So lets break it down into several different parts that may (or may not) be important:
Skin Incision Size
This is probably not important, and in fact, may be in some ways harmful. If the incision is too small, the first problem is that the surgeon may stretch or tear the skin, damaging it and leading to a higher risk of infection or a scar that does not heal as well. When you think about it logically, preparation of the bony surfaces is probably much more painful than the skin incision. Second, a limited skin incision may interfere with the surgeon’s ability to see and perform the procedure safely. It could lead to a higher risk of putting the hip or knee components in the wrong alignment or breaking one of the bones during component insertion.
Hence, I prefer a common sense approach. I make an incision that is large enough to perform the procedure safely but small enough to not cause unnecessary damage to the soft tissues. While I start with what many would consider a smaller incision, I make it larger if needed to perform the procedure safely. In patients who are thinner, smaller and more flexible the incision is usually smaller. In patients who are larger, heavier, more muscular or stiff, the incision may need to be larger. I still like perform a relatively small incision, however I just don’t think it is the most important part of achieving our stated goals of a safe procedure with a fast recovery and minimal pain. In general skin incisions are in the range of 4” to 8”.
Surgical Approach
Another common question. Please see more information under each specific procedure. In general there are several generally accepted ways to expose the hip and knee joint with the scientific data showing few important differences between them. They all have advantages and disadvantages.
Patient Education
Thorough preoperative education is probably among the more critical parts of a rapid recovery. If patients know what to expect, they have less anxiety and a faster recovery. Similarly, patient expectations are important and patients with a positive attitude generally recover more quickly!
Anesthesia
This is probably among the most important parts of a quick recovery with minimal pain and side effects. Please see individual procedures for more specifics on the type of anesthesia used.
Pain Medications
Again, this is probably quite important and the goal of our perioperative pain regimen is to use several different medications together, to make patients comfortable while minimizing side effects such as nausea and constipation.
Physical Therapy
Early ambulation and good physical therapy after surgery is a key component to a quick recovery. We do our best to get people out of bed (safely) and walking as fast as we can after surgery.
So what is the bottom line?
Well, I think a rapid recovery is achieved by a combination of things. It is not just the skin incision, the surgical approach or any of the other things listed. It is a comprehensive approach to care to achieve our stated goals; a safe procedure that minimizes the risk of complications with excellent pain control, minimal side effects and a rapid recovery.
How long before I can walk?
Our goal is to get you up and walking as soon as it is safe to do so after surgery. In some cases this will be the day of surgery and in others, it will be the morning after.
How long will I need to stay in the hospital?
To be honest, it depends! Factors to consider include your general health, if you have a good support system at home and how well you are able to tolerate postoperative pain.
For some of our healthier patients, we offer procedures at a surgery center and can avoid the hospital completely. If you prefer to be in the hospital, many procedures can be done with a short hospital stay. For patients with more complex medical problems, a three day stay in the hospital is more appropriate.
For more information, please visit our Outpatient Hip and Knee Replacement page, North Shore Surgical Suites page and Munster Specialty Surgery Center page and Rush Oak Brook Surgical Center.
Can you tell me about surgery at the Munster Specialty Surgery Center?
Dr. Della Valle performs outpatient hip and knee replacement at Munster Specialty Surgery Center in Munster, IN. Please click here for more information on outpatient procedures and the center in Munster, IN.
Can you tell me about surgery in Pleasant Prairie WI at North Shore Surgical Suites?
Dr. Della Valle performs outpatient hip and knee replacement at North Shore Surgical Suites in Pleasant Prairie, WI. Please click here for more information on outpatient procedures and the center in Pleasant Prairie, WI.
What type of anesthesia is used?
At Rush University Medical Center you will have spinal anesthesia. The anesthesiologist will give you some mild sedation and then perform an injection into your lower back that will make you numb for the operative procedure. If you are having knee surgery, you will also get an injection into your thigh (a nerve block) to help with pain after surgery.
This type of anesthesia provides not only great pain control, but is also associated with less bleeding at the time of surgery and may lower the risk of blood clots after surgery.
If you have severe arthritis of your spine or have had prior spine surgery this may not be an option for you. Please ask us if this is a concern, and we can arrange to have you see our anesthesia colleagues prior to surgery.
If you are having outpatient hip or knee replacement surgery at Munster Specialty Surgery Center, Rush Oak Brook Surgical Center, or North Shore Surgical Suites in Pleasant Prairie, WI the techniques are somewhat different so that you will be able to leave the facility comfortably and safely within a few hours of your surgical procedures.
Will my muscle be cut at the time of my hip or knee replacement?
This is a common question and understandably causes much confusion for patients. As far as I can ascertain, it is impossible to perform a hip or knee replacement without some damage to the surrounding muscles; whether they are cut of not is probably not important. Interestingly, when you think about it, there may be MORE potential for muscle damage if the surgeon uses a smaller incision and has to “force” things to get the job done. Our goal as stated is to provide you with a safe procedure, minimal pain and a faster recovery. We always do our best at the time of surgery to avoid unnecessary damage to the surrounding soft tissues but I don’t think that it is possible to perform a hip or knee replacement without detaching or cutting some muscle. Please see the articles below for some more information on this topic.
Journal Article: Anatomy of the extensor mechanism in reference to quadriceps-sparing TKA »
Why do you recommend against going to a rehabilitation facility after surgery?
Ideally, our preference is for patients to go home after surgery. Even patients who live alone can oftentimes be safely discharged to home. Most of the literature suggests that inpatient rehabilitation stays are associated with a higher risk of complications (particularly infection) and higher costs.
https://www.arthroplastyjournal.org/article/S0883-5403(17)30071-2/fulltext
https://www.arthroplastyjournal.org/article/S0883-5403(17)30280-2/fulltext
https://www.arthroplastyjournal.org/article/S0883-5403(15)01099-2/fulltext
https://www.arthroplastyjournal.org/article/S0883-5403(18)30010-X/fulltext
https://insights.ovid.com/pubmed?pmid=29342059
I have diabetes. Will this affect my surgery?
The short answer is “yes”. Diabetes has been shown to be a risk factor for infection as well as blood clots after surgery. To minimize your risk it is very important to control your blood sugars carefully both prior to and immediately after surgery.
At the time of booking your surgery, we will obtain a blood marker called “hemoglobin A1C” which is a marker of your blood sugar control over time. If this is not in a safe range, your surgery may be delayed to allow you to work with your primary care doctor to get your diabetes under better control to decrease your risks for surgery.
I am overweight. Will this affect my surgery?
Yes, in general people who are overweight have been shown to have a higher risk of problems and complications after surgery. In general we use something called the “body mass index” to gauge your risks. Patients with a body mass index of over 40 are at greatest increased risk and those risks are even greater if your body mass index is over 50.
We understand that weight loss with an arthritic joint is difficult. While healthy weight loss can be helpful (generally considered as one to two pounds per week), it is important to maintain healthy nutrition. We routinely asses nutrition, and if you are malnourished (yes people can be overweight and malnourished) your surgery may be delayed. Please ask us for more information on healthy weight loss and nutrition. The prevention center at Rush is an excellent resource for healthy weight loss. Rush also has several experts on weight loss surgery which may be appropriate in some cases.
Journal Article: Obesity and total joint arthroplasty: a literature based review »
How long will my replacement last?
This is a common question and concern, particularly for younger patients. To be honest, it is hard to predict but a good general guideline is the risk of failure is about 1% per year. That means at 10 years after surgery 90% of patients should have a hip or knee that is still working well.
While many patients are most concerned about their replacement “wearing out”, that is only one reason why a hip or knee can fail. The data actually suggests that infection is the most common cause of failure after knee replacements done in the United States and dislocation is the most common cause of failure of a hip replacement.
Where do you perform surgery?
Dr. Della Valle operates at Rush University Medical Center in Chicago, IL, Munster Specialty Surgery Center in Munster, IN, North Shore Surgical Suites in Pleasant Prairie, WI and Rush Oak Brook Surgical Center.
If I have arthritis of both hips or knees, can I do them both at the same time?
Most of the literature suggests a higher risk of complications and death if both joints are replaced at the same time. Hence, I prefer to perform them one at a time. If you need both joints replaced, they can generally be done two to three months apart.
How long will I be in the operating room?
Most of the procedures take between 90 minutes and three hours to perform, depending on the complexity of your procedure. However, the total time in the operating may be more as it takes time to perform the anesthesia and position you for the procedure.
I am not interested in surgery and want to explore non-operative treatment for my arthritis such as an injection into the joint and the use of medication and physical therapy. Should I come in to see Dr. Della Valle?
We have several partners who are focused on non-operative care and, ideally, patients are encouraged to see those physicians first. You will be able to get an appointment to see them more quickly and this is the focus of their practice. We are happy to see patients to discuss both surgical and non-surgical options, however, if you are sure that you do not want surgery, we do recommend seeing one of our partners first.
Will I be asked to participate in any research studies?
Yes, we have numerous studies going on that are helping us further understand joint replacement. Our goal is to use the data to improve post-operative outcomes for future patients. During your visit with us, we may discuss our research and request your participation.
Are there any questions I am forgetting to ask?
Probably the most important question you should be asking is how many procedures the surgeon performs annually. Most of the data that looks at the risks of complications (which most patients want to avoid) suggests that surgeon and hospital volume are both important in lowering the risk of complications and problems. This is no guarantee, but it does “stack the odds” in your favor. Dr. Della Valle has performed more than 9,000 hip and knee procedures and Rush performs thousands per year.
Unfortunately complications are inevitable. Much of my own research has looked at the diagnosis and treatment of complications after surgery and if you have a problem after surgery, our goal would be to recognize and treat it as quickly and effectively as possible.